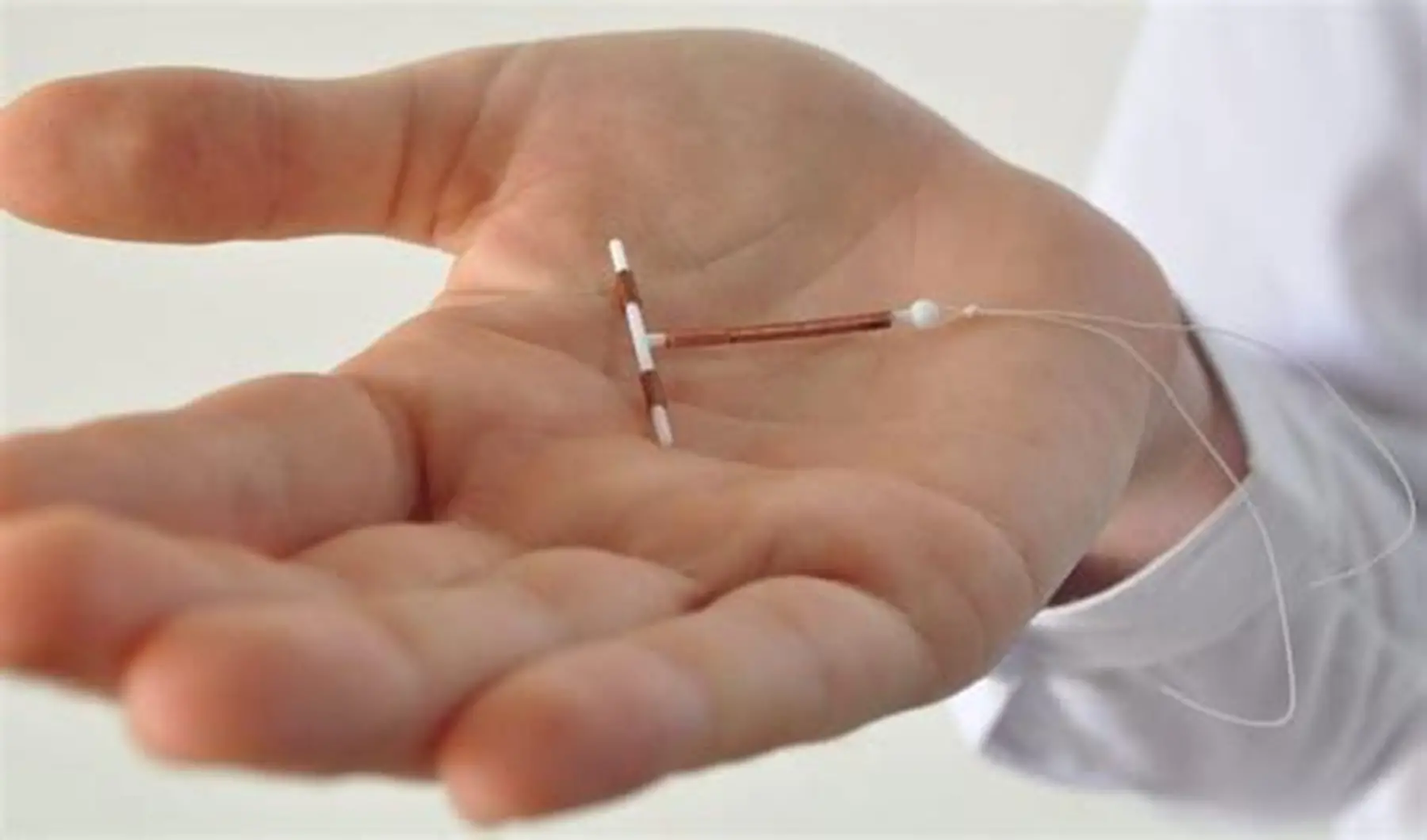
IUDs are also touted as among the most effective types of reversible birth control, with both hormonal and copper versions providing greater than 99 percent efficacy. These small, T-shaped devices are placed within the uterus and remain quiet in the background for years. But again, like most things in life, they’re not flawless. Though uncommon, it is possible to conceive with an IUD.

If pregnancy occurs with an IUD, it generally indicates that something went slightly wrong. The device could have moved out of position or even come out—expulsion, they call it—and this occurs in around 2 to 10 percent of situations. If you don’t realize that it’s no longer there, your risk of becoming pregnant rises. Occasionally, the IUD could be out of date or, with hormonal IUDs, not fully effective yet if you didn’t use backup birth control the first week after insertion. Copper IUDs begin to work immediately.

If you suspect there’s even a remote possibility that you could be pregnant and have an IUD inserted, don’t freak out—but don’t delay. Order a home pregnancy test or go see your doctor to confirm. If pregnant, it is important to get medical assistance early.

One of the main issues is ectopic pregnancy, where the growing egg penetrates outside the uterus, usually in a fallopian tube. This is dangerous, possibly deadly unless caught early.

Your physician will first check whether the pregnancy is in the uterus (intrauterine) or ectopic. If the pregnancy is in the uterus and appears to be available, your practitioner will probably recommend IUD removal. Its presence raises the danger of miscarriage, infection, and preterm labor.

Studies show that the danger of miscarriage is about 40 to 50 percent higher when the IUD is left in place. While there is always some increased risk even once it has been removed, it drops significantly.

There are risks to think about as well. These include infection, like chorioamnionitis, which attacks the placenta and amniotic fluid, and placental abruption, a risk condition when the placenta detaches from the uterus too soon. This causes too much bleeding and pregnancy loss. If you have a hormonal IUD, it will continue to release progestin into your uterus during pregnancy. While it is not exactly clear how this affects an in-utero-developing fetus, some animal research has raised concerns about birth defects.

The symptoms of an IUD pregnancy are generally the same as any pregnancy: missed menstrual period, tender breasts, nausea, fatigue, and perhaps some spotting. But if you have sharp pelvic pain, sudden bleeding, aching shoulders, or experience dizziness or clamminess, these can be signs of an ectopic pregnancy, and immediate medical intervention is needed.

Removing an IUD during pregnancy is typically an easy procedure if the strings are still visible. If they’re not visible, your provider may have to use ultrasound or special instruments to take them out. Rarely, if the uterus is too large to safely remove the IUD, it would have to remain in place until delivery. That’s not preferable, but sometimes it’s the best option.

Emotionally, learning you are pregnant with an IUD can be very disappointing or puzzling. It’s not what the majority of people anticipate, and in the event the pregnancy is not viable or is ectopic, it can be a feeling of loss. Counseling from your doctor, counselor, or reputable organizations can assist you in processing the emotional aspect as much as the physical.

Ultimately, IUDs are among the most effective birth control methods available, but no method is entirely foolproof. If you have an IUD and something doesn’t feel right—like if you can’t feel the strings, you’re bleeding when you shouldn’t be, or experiencing heavy cramps—it’s a good idea to check in with your provider. A little extra vigilance can make a big difference in keeping your health and peace of mind intact.